Hormone Therapy a Historical Perspective
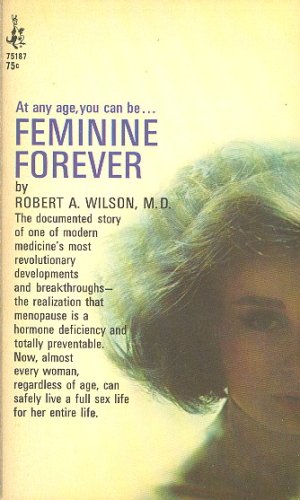
Feminine Forever!
In 1966 Robert Wilson MD published his book Feminine Forever promoting the use of estrogen to treat menopause symptoms and hot flashes. He wrote, “untreated menopause robbed women of their femininity and doomed them to live the remainder of their lives as mere remnants of their previous selves.” He called women castrates. In his opinion reversing body changes in middle-aged women restored sexual function. Reversing these changes would allow women to look feminine again. Women responded to what Dr. Wilson said by speaking even more about menopause. They said that ageing is a complex process involving not just estrogen but other factors. There was concern that Dr. Wilson was taking advantage of a most susceptible group of women when he promised a cure for menopause.
WHI Findings
Declining estrogen levels have interested doctors and patients for many years. Conjugated Equine Estrogen (Premarin), introduced as early as 1942 offered relief for menopause symptoms, most notably hot flashes. In the 1970’s women stopped taking Premarin because of an increase in risk for cancer of the endometrium (lining of the womb). Hormone therapy (HT) use has slowly increased since the 1980’s when long-term research showed the protective effects against osteoporosis (brittle bone disease) and possibly heart disease. Improved treatment schedules and different ways of delivering the hormones have increased its use.
Women’s Health Initiative (WHI) – Inclusion of Women in Research Studies
Participants in prevention and treatment studies of diseases were mainly white men. In order to receive funding for research The Office of Research on Women’s Health strengthened the policy to require the inclusion of women and minorities in clinical research where appropriate. This, therefore, made it possible for the National Heart Lung and Blood Institute to receive funding to sponsor the WHI study to address major health issues causing health problems and death in postmenopausal women.
The WHI health project to study women’s health in the United States began in 1992. It was to end in 2007. It is one of the largest projects to study women’s health in the United States. More than 161000 postmenopausal women between the ages of 50-79 (average age 63) enrolled at 40 clinical centers. The goal of this long-term national health study was to look at ways to prevent heart disease, breast cancer, bowel cancer and osteoporosis in postmenopausal women. These chronic diseases are the main causes of death and disability in older women.
The abrupt ending of the Estrogen Progestogen (EP) arm of the study in July 2002 was another milestone in the history of the use of postmenopausal hormone therapy. This decision left millions of women and their doctors afraid, confused. They discontinued taking hormones because of findings of increased risk of stroke, blood clots, coronary heart disease and breast cancer when taken for more than 5 years. There was the possibility of women getting dementia.
At the end of the study less women developed bowel cancer and cancer of the lining of the womb. There were less hip fractures and diabetes. Furthermore it was possible that less women developed breast cancer. Taking estrogen alone reveal. There were fewer deaths overall. The conclusion was that there was more harm than benefits.
The North American Menopause Society Recommendations
The North American Menopause Society Board of Trustees put together a Hormone Therapy Advisory Panel to report on updates. It presented clinical recommendations for hormone therapy use in women entering into the menopause and post-menopause. The primary indication for hormone therapy use published in the report September 17, 2003 is the treatment of moderate to severe menopause symptoms. Hot flashes, sleep disruption, vaginal dryness, painful sex and thinning of the vaginal lining are among the recommended symptoms. Women age 65 and older are at risk for heart disease and dementia. Hormone therapy is not recommended for prevention of these conditions.
Most noteworthy is the fact that several hormone products have the Food and Drug Administration’s (FDA) approval. Even more, the FDA approved hormone therapy for postmenopausal osteoporosis prevention. Women who wish to take hormone therapy for a longer period of time can certainly look at other product options weighing the risks and benefits of each. The panel acknowledged that the absolute risks published regarding hormone therapy use are small. There is a need for future research to continue studying the positive and negative effects of hormone therapy and the mechanisms by which they occur.
Where do we go from here – Hormone Therapy Update
We are still learning from the women who participated in the study. Researchers are continuing to look at the information collected. They are discovering more information about hormone therapy and heart disease. In 2017 the North American Menopause Society updated their Hormone Therapy Position Statement. In my experience, I find that women want to arm themselves with the right information. They are seeking information to prepare for the changes that occur in menopause and beyond. Women along with their healthcare providers want to be able to make an informed decision as to what management strategy is best using the best available scientific information. They seek to increase benefits and decrease risks.
Helping women to decide
The bottom line is this, risks of hormone therapy are not the same for every woman. Risks are lower when women start hormone therapy within 10 years of menopause, before age 60 years. Above all, women who had a blood clot or is at risk of having one should not take hormone therapy. Consequently, some women who test positive for the BRCA breast cancer gene remove their ovaries. Removal of the ovaries is an attempt to lower breast cancer risk. Most importantly, BRCA-positive women who removed their ovaries showed no increase risk while using hormone therapy. Taking estrogen alone may reduce breast cancer risk.
Using estrogen plus progestogen treatment in women who still have their womb for the short-term carries no significant increase in risk. It is important to personalize treatment for each woman. Assessing risks and benefits are even more important for continuation of hormone therapy. Hormone therapy can be considered for continuation after age 65 for ongoing hot flashes, quality of life issues or osteoporosis prevention. Low dose vaginal estrogen is recommended for symptoms in the vaginal and bladder areas not relieved with over-the-counter or other treatments.
If the only tool you have is a hammer, you tend to see every problem as a nail – Abraham Maslow
